The chronic illness debate is more mainstream – But still mysterious
One effect of the coronavirus pandemic has been to normalize a debate about mysterious chronic illnesses that previously hovered at the fringes of American public discourse. If you followed this debate closely – excruciatingly closely, in the cases of the mysteriously sick and their loved ones – you noticed it breaking into the mainstream occasionally: a magazine feature here, a celebrity memoir there. But not in the consistent way of 2020-22, when the debate about Covid-19’s baffling and debilitating “long haul” symptoms became an important spoke in our larger wheel of pandemic-era arguments.
Ideally, this heightened interest in chronic suffering would be a simple good: It would yield more research, more medical creativity, more sustained analysis of why certain sicknesses linger or recur for a meaningful minority, even as they’re easily resolved for the majority.
This is happening to some extent. But having an issue or debate go mainstream also makes it captive to partisan polarization. The experience of long-term Covid symptoms doesn’t appear to be distributed in any ideological pattern. But beliefs about long Covid – its reality, its importance, whether its victims need a cure or a counseling session – often show up (on social media especially) as part of a larger package of ideological assumptions, another tribal signifier pitting masked-up hypochondriacs against vaccine-denying cranks (to invoke each tribe’s stereotype of the other).
I tried to push back against this tribalization in a column last spring, which made the case that you can believe in the reality of long Covid without also believing that it requires a permanent emergency mentality or China-style zero-Covid aspirations.
But a different way to escape the pull of tribalism is to consider cases of chronic illness that remain well outside the patterns of the coronavirus era. Cases in which there’s no collective experience involved to help the strangeness make some sense. (Or, if you’re skeptical, to condition suffering people to reach for a culturally scripted explanation.) Cases that reemphasize the “mystery” part of mystery illnesses, the irreducible challenges of treating sicknesses that fall outside existing medical consensus.
Here’s a compelling account of one such case, written for NowThis News by Kris Newby about a teenage boy in the Midwest, Michael – a pseudonym – whose life fell apart in the span of months, carrying him from early adolescent normalcy to apparent mental breakdown:
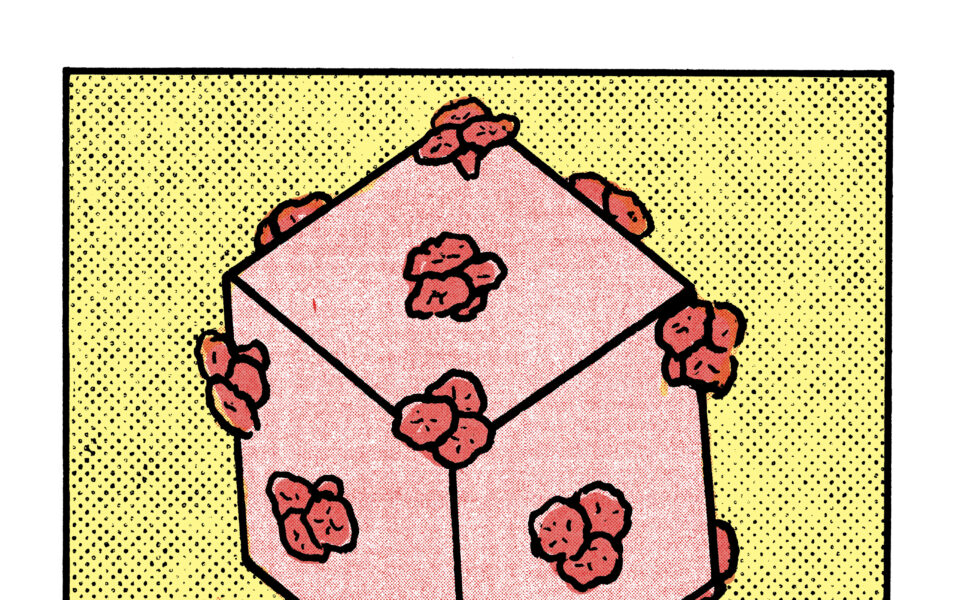
Michael’s parents would observe him having conversations with imaginary beings or his comic book figurines. Then, during one psychotic episode in the family’s basement, Michael told his parents that he was no longer human. He announced he was becoming “Swamp Thing,” a green, plant-covered comic book monster – one of the characters from the posters in his room. “I can feel the vines on my skin,” he said, as he tried to pull them off his shoulders and arms.
In this phase of his illness, Michael also grew convinced that his yellow tabby cat and his father were possessed by demons. The cat would telepathically threaten him, sending him running and screaming through the house, looking for someplace to hide. Michael would then curl up in the fetal position, sobbing.
Newby’s story describes how Michael was diagnosed with schizophrenia, institutionalized in a Texas clinic and treated with a battery of antipsychotic drugs at ever-higher doses. (One doctor reportedly told Michael’s mother that he needed to be given clozapine, an antipsychotic of last resort, “until he drools.”)
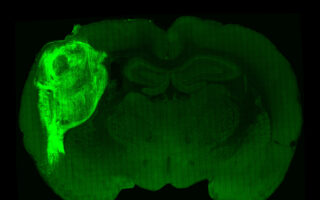
But none of these treatments seemed to yield stability or improvement. So Michael’s father took a step that we’re all supposed to regard as terribly reckless and did his own research on the internet. This led the family first to a diagnosis of pediatric acute-onset neuropsychiatric syndrome, or PANS, a catchall for symptoms linked to some uncertain trigger like an infection, and then via various twists and turns to a specific bacterial culprit, Bartonella, known as cat-scratch fever for its association with feral cats and fleas, whose treatment with a complex of antibiotics eventually restored Michael to sanity and health.
I hope you’ll read the full story because I want to make four observations about its details. Each observation is also linked to the story I tell in my recent book, “The Deep Places,” about my own mystery illness experience – which turned out to be Lyme disease along with Bartonella, which is carried by ticks as well as cats and fleas. But all of them generalize beyond the particular overlaps between Michael’s case and my own.
The mysteriously ill don’t necessarily have a bias against psychiatric diagnoses. A certain kind of skeptical commentary tends to assume that the chronically ill are unreasonably resisting a psychological diagnosis, because it seems stigmatizing or insulting. (This is a recurring theme of skeptical reportage on long Covid patient advocacy, for instance.) No doubt sometimes this is true, and there are certainly case studies of people finding relief from chronic pain and suffering using cognitive techniques.
But the stereotype of people refusing to accept a mental health diagnosis seems like an odd fit for contemporary American society. From our ever increasing rates of antidepressant prescriptions to our therapeutic style of spirituality, neither our medical system nor our culture writ large seems meaningfully resistant to psychiatric diagnoses or mind-body treatments. If anything, the medical system’s bias often runs the other way: If your blood tests come back negative or your symptoms don’t yield a simple diagnosis, you’re very likely to be told to consider seeing a mental health professional, and most people who like and trust their own doctors (which is to say, many people) will follow that advice.
In Michael’s case, this was particularly natural because the psychiatric symptoms preceded the physical ones; he suffered hallucinations initially, and then headaches and chest pain kicked in later. But even when you only have physical symptoms, as I did when I first fell ill, the psychiatric explanation can be reassuring rather than offensive, both because it seems so culturally familiar at this point, and simply because it is an explanation for something you yourself can’t explain, buttressed by authority and promising eventual relief. (The outsider doctors I saw for my eventual Lyme treatment, for instance, took it as a given that many of the people coming to them would have spent months or years on various psychiatric medications.)
In my own case, this reassurance didn’t last because both psychiatrists I saw told me (to their immense credit) that they didn’t think my physical symptoms could be explained by a mental health disorder. But even so, there was a period of months when I was reading books about anxiety disorders, telling even casual acquaintances that I was suffering a nervous breakdown, taking a battery of drugs – antidepressants, Xanax, sleeping pills, more – and generally trying to talk myself into believing that the stabbing pain in my chest had to be a dagger of the mind … because that was at least a diagnosis, a potential path when every other path was too obscure.
Sometimes there’s no escape from becoming your own doctor. The happy ending to Michael’s story notwithstanding, it’s a fraught thing to wander strange paths on your own, seeking out a diagnosis via research on the internet: Witness, say, the recent boom in teenagers self-diagnosing mental health disorders via TikTok. (Though note, again, that none of these teens are resisting a mental health diagnosis; quite the reverse!)
But with illnesses that don’t fit into normal patterns, there often really isn’t any other alternative, because you – you the patient, or you the caregiver – have to choose for yourself between competing medical theories and explanations. As Michael’s story makes clear, Does my kid suffer from PANS? is not a question our existing medical system can simply answer on its own, because doctors disagree about whether PANS is an appropriate diagnostic category. The same goes for his Bartonella diagnosis: As Newby writes, there are running debates about every aspect of the condition, including how to test for it and how to treat it, to say nothing of the super weird “Jarisch-Herxheimer” reaction – the temporary worsening of symptoms under treatment – that was part of Michael’s response to his antibiotic regimen.
And something very similar is true for people going through a long-haul Covid experience today. They may have to make decisions for themselves in advance of the science, because agreement on what the science says may not come in time to save them.
Illness undermines ideological frameworks. What kind of story is Newby’s article? Well, it appears in NowThis News, a left-leaning outlet, at a time when late pandemic debates have coded belief in the seriousness of chronic illness as the left-wing position and greater skepticism as the right-wing position. So it must be a left-wing intervention.
But wait: It’s a story about a prayerful Christian family and a father who threw himself into his own private medical research, embraced a controversial diagnosis in defiance of the doctors who were initially treating his son and found help via a facility, the Sancta Familia Center for Integrative Medicine, that’s “infused with Christian values.” So, clearly, it must be a right-wing critique of the liberal medical establishment; the only surprise is that Michael’s parents didn’t give him ivermectin.
The reality is that you just can’t fit these experiences into ideological boxes. Absent a direct encounter with a mystery illness or its outré treatments, it’s easy enough to assume blue-state hypochondria or red-state science denial, as your priors prefer. But inside the country of illness, those categories turn out to be brittle, simplified and insufficient to the actual experience itself.
You can’t take the “mystery” out of “mystery illness.” Part of Michael’s story is scientifically straightforward: Boy gets devastating infection, infection is misdiagnosed and then finally uncovered and treated successfully. But part of the narrative interest in Newby’s article lies in the weirder stuff. The fact that the family house cat was a consistent locus for Michael’s hallucinations long before cat-scratch fever entered the discussion, threatening him and chasing him and telling him to kill his sibling. The way he latched onto the analogy to the comic book character Swamp Thing, describing a sense of symbiosis between his own human body and some other organic force at a time when his doctors were dismissing the idea of infection. The fact that his worst reaction to the treatment ended and his psychosis broke between Good Friday and Easter Sunday.
You can read each of these elements in different ways. As essentially random details that happened to lend themselves to the kinds of stories humans need to tell to make sense of our essentially random suffering. Or as examples of undiscovered mind-body entanglements that enable the subconscious to intuit things that doctors haven’t figured out. Or even as trace elements of the supernatural.
However you read them, though, they’re all examples of how a mystery illness is inevitably an “edge” experience, pushing the sick person into territory that’s just fundamentally weirder than the secular and scientific everyday. Which then becomes its own challenge when the time comes for reentry. You need to tell a story that makes sense back in the normal world, that normal people will find credible and plausible.
But you also have to be honest about just how much stranger the world looks from the edge, the beyond, the places underneath.
This article originally appeared in The New York Times.