Normalcy could return in autumn

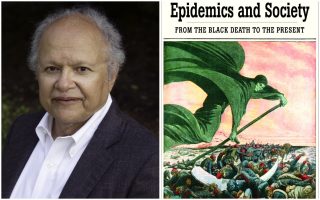
Dr Anthony Fauci, US President Joe Biden’s chief medical adviser, who gave this interview to Kathimerini, is the best known expert on the pandemic – not just in the US but worldwide – having worked alongside all the presidents since Ronald Reagan and then playing a leading role in tackling AIDS and later Ebola.
In the case of Covid-19, his mission was much more difficult. He had a president who, at first, did not believe that the virus was a real threat; he had to deal with conspiracy theories, the refusal of many of his compatriots to wear masks, and even threats against his life.
When I asked him about it, Fauci said that he managed to get through it because he focused on his job and always kept in mind that the enemy is the virus.
In this interview, however, you will find answers to a number of key questions that concern us all. How dangerous the Covid variants are; how safe the vaccines are; if there will be an effective treatment for Covid; when we can say we have won the battle against it; when we will be able to stop wearing masks; when we will be able to travel again; and how we can prepare for the next pandemic.
Fauci has an amazing way of explaining complex scientific issues. That is why he is the most recognizable official, with immense credibility on public health issues. I confess that I had wanted to do this interview for many months because this man looked like a real hero as he handled an unprecedented crisis in surreal conditions.
I was impressed by a documentary about him before the current pandemic. It showed him, in full personal protective equipment, examining a patient with Ebola, at a time when it was considered the most dangerous, deadly virus. They asked him why he did it and if he was scared. He replied that he was scared and that his wife almost divorced him because of the risk he was taking. But he added: “It was important for me that my colleagues see that I, as the team leader, took the risk of examining the patient. Leadership comes at a cost.”
How concerned are you about the different variants of the virus? Is it just more transmissible or is it also more deadly, more dangerous? What’s your assessment?
Well, there are a number of variants that we’re dealing with. We take all of them seriously. Some are of less concern than others whereas some have a degree of capability that makes one concerned, and want to make sure that the vaccines that we have address them. For example, the variant that is dominant in South Africa is called the B1351 variant. We know that not only does it spread rather efficiently, but when you look at the protection that you would expect from some of the monoclonal antibodies and from the antibodies that are induced by the vaccine, some of the effects of the monoclonal antibodies are diminished, if not essentially eliminated. But the antibodies that are induced by the vaccine are diminished by about five-fold in their ability to contain the virus. That is the sobering news. However, what we do know is that some of the vaccines – for example the vaccine that is the M-RNA from Moderna and from Pfizer and the J(ohnson) and J(ohnson) vaccine – when you look at them, even though it diminishes somewhat the capability of the vaccine, the vaccines still protect very well from very severe disease such as hospitalizations and deaths. There are other vaccines that may not be as effective against that variant. We have other variants, for example, the 117 that started off in the United Kingdom. That one we know has a clear capability of spreading more efficiently from person to person. However, the vaccines seem to do pretty well against that, even though it spreads. The Brazilian variant is very similar to the variant in South Africa. And finally, we have a few variants in the United States – one in California, which is the 427/429, one in the New York City metropolitan area, which is the 526 – that are giving us a problem because they spread pretty easily and they do diminish somewhat – not a lot, but somewhat – the effect of the vaccines. So, the bottom-line summary is we have got to take them very seriously. Some of them are more problematic than others. But we have got to continue to do surveillance, namely do genetic and genomic sequencing of the strains that are in the individual country. I would be very surprised if Greece did not have their own variants that they need to make sure that they look out for, because they may need to make sure that the vaccines that they’re using are actually effective against the mutants.
There has been a lot of discussion about the potential side effects of the vaccines. Based on what you have seen so far, what is the level of your concern?
The level of my concern is minimal. And the reason I say that is that in the vaccine trials that we did in the United States, with the m-RNA from Pfizer and from Moderna, they were really highly efficacious – 94% to 95% – but the reactogenicity is minimum. After the first dose, you get a feeling of achiness in your arm that lasts for about 24 hours. There is more reactogenicity after the second dose. And that occurs 21 days later with Pfizer and 28 days later with Moderna. What happens after the second dose is you can get a feeling of fatigue, of achiness, of some chilliness, and maybe a little bit of a fever. That only lasts, in most people, for about 24 hours – some people a little bit longer, but for the overwhelming majority of the people they last for 24 hours and then it goes away spontaneously and you’re fine.
Would you have the Sputnik or the Chinese vaccine?
Well, the data that I have seen from Sputnik look pretty good. I do not have as much information on the Chinese, because the Chinese have two or three different vaccines. So, I have not followed carefully the relative efficacy of them, but the data that I’ve seen from the Russian one looks pretty good.
There is a lot of debate about whether, in some cases, when countries are on the brink of another wave, only one dose of the Pfizer should be given, or some other vaccines. What is your view on this?
No, I do not like that approach for the following reason: We have shown that – take the Pfizer vaccine for example – after the first dose you get a modest amount of antibody level, that is good enough to maybe protect 52% as opposed to 94%-95%. It does protect – well 52% is not bad. We do not know how long it lasts. When you give a boost, the level goes up 10 times higher. When you are dealing with the variants, the variants diminish the efficacy by maybe fivefold down. So, if you are starting off at a very low level with a single dose, it may be good against the regular virus, but when the variant is around, it could fall below the level of protection. So even though it has the advantage of giving more vaccines to more people right away, it has the disadvantage that you do not know how long the protection lasts. And you could get into trouble if you are dealing with variants in Greece as opposed to the standard virus. So, the science tells us that the least risky thing to do, and the more confident we are, is a single dose, followed by the second dose.
I want to ask you about herd immunity, because I remember you saying a few months back that you would be comfortable at the 60% level. Now you say that the threshold is about 80%. What has changed? What is your final assessment?
We have to realize that it is just an estimate, because the only way you know what the exact level is, is when you get there, and then you fall below, and infections occur. So, we know exactly what it is with measles because we have decades of experience with measles. We know that the level of herd immunity is about 90% of the population. Once you get into the 80s, as we have seen in our own country when certain pockets of people in the community got below a certain level, we had outbreaks. With regard to Covid-19, we can only estimate what it would be and the more we’re looking at the degree of spread and the level of efficacy of the vaccine, we think it’s about 70% to 85% of the population. Somewhere between 70% and 85%. But I must caution you, that still is just an estimate.
Do you think there might be a cure for Covid? We have heard about some promising research in Israel, for example. Do you see any potential in all this?
I think that just the way we developed good drugs for HIV, by targeted drug development, and just the way we developed good drugs for hepatitis C, I think with a good investment of time and resources that we will ultimately have very good drugs for Covid. But I do not think that is going to be immediately. I think it will take a little while.
When do you think D-Day will be in terms of the pandemic? When will we really be able to say that this is all over, when we can go out into the streets and celebrate?
That is difficult to predict for the following reason. It would depend on the individual country. This is a global pandemic, which requires a global response. And one of the things is that until we get vaccine available globally, Greece could do a good job in getting their people vaccinated and suppressing the level of virus to a low level. The United States could do a good job, the European Union, the UK, Australia, but if there are still parts of the world that do not have the capability of vaccinating their people and suppressing the virus there is always the danger that new variants will come and reseed Greece and reseed the United States. So, I think we can get it down to a very low level. I hope that by the end of the fall and the end of this year, 2021, that we will be able to approach a significant degree of normality. Maybe not absolutely normal, the way it was before all of this happened. But I think starting with the fall of this year we will gradually be able to do some of the things that we are not doing now – such as sports, such as indoor dining, such as entertainment, the things we have not been able to do. I would hope so. That will depend on making sure that we continue to adhere to public health measures and only gradually pull them back and that we successfully vaccinate a substantial proportion of the population.
But I imagine that we will be wearing masks for a while longer, right?
Yes, I believe that until the level of infection gets very, very low, almost non-perceptible, I think we will have to wear masks. I think as more and more people get vaccinated, they would have the opportunity in their own homes, with friends, with family, to be able to safely interact socially without a mask. But that would likely be in very confined situations like in your own home or in the home of a friend. But going out into society, I think it would still be quite a while where we will have to wear masks.
You know tourism is a big thing here in Greece. So, if a vaccinated American asked you whether he could come to Greece this summer, what would you say to him?
You know, it would depend on what the level of infection in Greece was. I mean, if the level of infection in Greece gets down very low and the Greek people get vaccinated, so that they can suppress these surges of infection, I think gradually travel would be allowable and would be advisable. Because everybody wants to get back to normal and many people, myself included, feel that one of the most beautiful places to go is Greece. So, I think people would want to do that.
Now, seeing you on TV all this time, it looked like a very surreal experience when you were working with the previous administration. I wonder whether it was, and how it felt to be squeezed between science and politics in such a brutal way.
It was very difficult. And the only way I got through it was to focus on the importance of what I needed to do. It would be to do the science and [focus on] the public health that protects, directly, the American people and then, by that extension, indirectly, the rest of the world. Because my job was to develop the vaccines, to develop the drugs, to be the public health spokesman. But you are right. It was very, very difficult because, as you know – and I’m sure you do in your position as a journalist – in the United States it is a very, very divisive society. One of the really difficult things to do is to carry out a successful public health endeavor when you have half of the country divided with the other half and public health measures take on a political connotation, as opposed to dissociating it completely from politics and just concentrating on pushing and pulling together. So, the only way you are going to get through an outbreak is by everybody being together in a common goal. The enemy is the virus. The enemy is not the opposition, politically. The enemy is the virus. And that is what we need to do, essentially join together against the virus.
There is a big debate here in Greece because we are experiencing a third wave. And there is debate about whether schools should open, whether retail stores should open, people moving around, and all that. What is your recommendation? What do you suggest?
Well, one of the things that you have to do is know what the level of the surge is, about what percent positivity testing is. You know, in the United States we have Blue Zones, Yellow Zones, Orange Zones and Red Zones. Blue is the test positivity from 0% to 9%, yellow is from 9% to 50%, orange is 50% to 100% and red is greater than 100%. So, if you are in the very, very far red zone, you have got to be very stringent with public health measures. You have really got to. No indoor dining, close the gyms, and things like that. If you get to a more modest [number] there are four or five things that you should do anyway. Uniform wearing of masks, avoiding congregate settings, particularly indoors, keeping physical distance, washing your hands very frequently. It really depends on the level of penetrance of infection in the community to determine what level of restriction you are going to put on the country.
I heard President Joe Biden the other day saying that most of the US population is going to be vaccinated by May.
No [laughs]. He said, by May we will have enough vaccine to vaccinate everyone. The logistical challenge of getting everybody vaccinated will likely take multiple months more. We will have enough vaccine by May, but if you want to get the 70% to 85% of the people vaccinated it likely will take well into the summer. Towards the end of the summer.
So, do you think everybody will probably be vaccinated by early fall?
Not everybody, because we have a lot of people in the country who do not want to be vaccinated.
Do you still have that?
We still have vaccine hesitancy, yes.
Europe seems to be lagging behind the US in terms of getting our logistics in place. Are we doing something wrong?
Well, it depends on what you are talking about. Logistics about vaccines or just logistics about the outbreak in general?
About vaccines.
About vaccines. Well, I do not think you are doing anything wrong. It is just that different countries have different capabilities. What President Biden has done is he has made this a very top priority: getting the vaccine into the arms of people. For example, he has created community vaccine centers, particularly in those areas that might be underserved by the healthcare system, which is generally very heavily weighted towards our minority populations, African Americans, Hispanics, and others. Next, he has put vaccines into the pharmacies to be readily accessible to people. Next, he has created mobile units to go into areas that are not easily accessible. And he has got a lot of people who are called vaccinators, people who will be doing the actual injecting into the arms of people. He has gotten our National Guard, our home military, he has gotten retired doctors and retired nurses to come out of retirement to help to administer. In the beginning, when he first took over, we did not have that in place and the administration was not as well organized as it is now where you have a very well-organized plan to distribute the vaccines.
You have dealt with AIDS, you have dealt with Ebola. Now you have dealt with this pandemic. Is the next pandemic going to be different?
I hope that this very difficult experience that we have all gone through will provide lessons that we have learned that will help us both in the preparation for and in the response to the next outbreak, whatever that might be. And one of the things we have learned from experience is that it is very difficult and generally impossible to predict what the next major outbreak is going to be. So, we have got to be prepared. We have got to have a good Global Health Security Network. We have got to have cooperation, collaboration and solidarity throughout the world because you never know where and when the next outbreak will occur.
And my last question is, if there is one moment, one episode, that really sticks out in your mind from this past year, what would that be?
One episode? You know, I think when we finally realized that we had a real problem in the United States, where the virus was spreading under the radar screen because we realized that a lot of it was spread by people who had no symptoms. That made it very, very difficult to track and do contact tracing, and, as you know, right now we have about 520,000 deaths in the United States, which was unimaginable a couple of years ago, to think that we would have an outbreak where more than half a million people died from an infectious disease. That statistic sticks out to me in a very painful way.